Lung cancer
Overview
Breast cancer, which has certain genetic predisposition, is now the most common cancer in Chinese women. Breast cancer mortality ranks sixth among cancer-caused deaths. According to the latest statistics, the number of new breast cancer cases in women reached 269,000 in 2015.
10% breast cancers are caused by genetic mutations, which have a 50 percent chance of being passed on to children, and other immediate family members of breast cancer patients also have high risk of carrying these genetic mutations. BRCA1 and BRCA2 are cancer suppressor genes that can repair damaged DNA. If mutation occurs in specific sites of these genes, the tumor suppressor protein will change and DNA repairing will be inhibited, which causes cells to accumulate harmful DNA damages and eventually leads to occurrence of such cancers as hereditary breast and ovarian cancer. For BRCA1 / BRCA2 mutation carriers, the risk of breast cancer increases significantly and the age of onset of breast cancer tends to be young.
Breast cancer gene detection is detection of breast cancer-related genes in samples of cancer tissue and peripheral blood through use of high-throughput sequencing platform. Through lung cancer gene detection, detection of genes associated with breast cancer and conventional chemotherapy for breast cancer and personalized medication guidance for patients can be achieved.
The Necessity of Genetic Testing
Scientific research shows that cancer is caused by genetic mutation in human body, which causes cells to lose its normal control function and thus proliferate wildly and eventually form a tumor. Targeted drugs specifically target sites where specific genetic mutations occur, kill tumor cells and do not kill normal tissue cells around the tumor. At present, FDA-approved breast cancer targeted drugs include herceptin, everolimus, lapatinib, papoxidil and so on. However, these drugs are only applicable to patients with some certain types of breast cancer.
Through use of multi-gene detection technology, targeted drug-related gene mutations in breast cancer patients’ tumor tissue/blood can be detected and analyzed, metabolism of commonly used drugs and mutations of multiple genes can be detected and reasonable selection of best targeted drugs, chemotherapy drugs and treatment programs can be achieved.
Testing Content and Medication Guidance
Through detection of 21 genes associated with breast cancer using high-throughput sequencing technologies, the characteristics of the tumor can be determined by observing the interaction between genes, thus the probability of recurrence of breast cancer and chemotherapy effect can be predicted. That is to say, through genetic testing, patients can learn whether or not his or her breast cancer will relapse, the probability of relapse and the necessity of postoperative chemotherapy.
|
Part of the genes for detection |
ABCB1 BRCA1 BRCA2 BRAF CDK4 CDK6 CYP19A1 CDH1 CCND1 EGFR ERBB3 ESR1 HER2 TSC1 PIK3CA NTRK1 TP53 PTEN |
|
Part of the targeted drugs |
Pani monoclonal antibody, Cetuximab, Sunitinib, Vanderbilt, Reggie, Quimeitidine, Dalafini, Gefitinib,Carbotinib, Sertini, Sorafini, Everolimus, Imatinib |
|
Major manufacturers |
Roche Betta Pharmaceuticals Co., Ltd Pfizer Novartis GlaxoSmithKline |
|
Notes |
The drugs listed here include FDA/CDFA-approved drugs and clinical trial drugs |
Applicable People
Breast cancer patients who expect to adopt targeted drug therapy
Screening for hereditary breast cancer, providing targeted treatment, and providing important reference information for relatives
Patients who need chemotherapy for breast cancer
Healthy people who are concerned about breast cancer
Clinical Significance
Genetic testing can help breast cancer patients select appropriate targeted drugs and can detect acquired drug resistance mutations.
Sample Requirement
Fresh cancer tissue: ≥60mg
Fresh percutaneous biopsy tissue: 2~3 needles
Paraffin-embedded tissue: 8~10 paraffin embedded tissue sections
DNA: DNA:concentration≥30ng/μL, 260/280≈1.8~2.0,gDNA≥1ug,cfDNA≥500ng
Peripheral blood: 10mL fresh peripheral blood
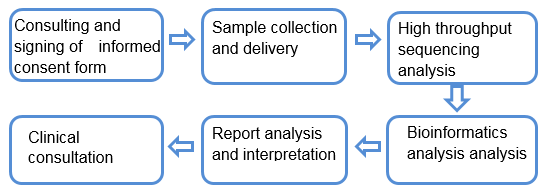
Service Process
- 上一篇:FAQ
- 下一篇:Breast cancer
